Street drugs are easier to get...
Why is getting the drugs I need such a project? Why do insurance companies like to make it difficult for people to get the medications they need on a daily basis. I know I'm not the only person with CF that runs into these issues. Since moving to CO I've had such insurance issues, Medicare does not cover everything, therefore I needed to get a secondary insurance. Even so, I'm still having issues! One of the main inhaled medications that people with CF need is called Pulmozyme. It's mucolytic, meaning that it helps thin the mucus. This is a drug that I need to take twice a day. Well medicare doesn't care and will only cover the drug for once a day...(what the shit is this!?!) Bull shit is what it is! One reason I think they do not cover 2x a day for 30 days is because it would cost them about $7,000....(eek!) Yes, my drugs are expensive. So before knowing that they only covered it once a day I was using the box of Pumozyme like I'm supposed to, twice a day. In doing so I have been running out quickly and calling in for a refill and then finding out I had to wait until a certain date for them to bill the insurance, therefore having to wait like a week or two for a new box...(lame llamas).
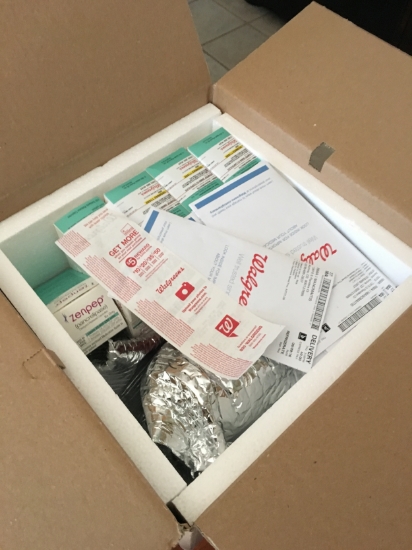
Sometimes several of my meds run out around the same time and last week there were four. Zenpep my enzymes. And then three inhaled meds, Duoneb, Pulmozyme and Perforomist. Luckily I've found a specialty pharmacy that is super versed with CF meds and insurance issues and they have been so amazing. They're buddies with the folks I see at National Jewish. Specialty pharmacies deal with some of the drugs regular pharmacies don't, they also deliver! The three drugs that came are quite pricey, but definitely not the most expensive of the CF meds out there. Of course I was doing the happy dance when they arrived. One, because they came the next day and two there was no copay, imaginary backflips in celebration! The specialty pharmacy is actually a Walgreens located in the Children's Hospital in Denver. They've been providing me with the meds that either take a while at the Walgreens close to me (about 4 minutes), or they just don't have. One of the meds that I totally spaced on while calling in the other meds to the specialty pharmacy was my albuterol inhaler, which I've been using more because of allergies. So I had to call it into the local Walgreens because it was the weekend. On Sunday I went to go pick it up, and of course it wasn't quick and easy. I was waiting in the drive thru for a while because apparently my insurance doesn't cover that brand of inhaler (pro-air) and it would cost $140...(ha! no thanks). So the pharmacy manager had to come over and tell me that they're going to try a different brand, and lo and behold a different brand was $0 copay! (yayayyyy!). The total of the four meds that is billed to insurance is $11,022.76 (oh my lanta!)
A few months ago the social worker at National Jewish told me about Health Well Foundation. This foundation is to help with the cost of copays. So Laima and I went on and I applied, it was quick and easy. They give you a list of all the CF meds they cover and you check off the ones that you are on. About a week or two later and in the mail came an approval letter and my Health Well card. All I have to do now is give the info on the card to the pharmacy and they should be going through that after running the prescription. The specialty Walgreens already had that info and used it with my prescriptions without any issues! Sometimes there is a god! A god of cooperation with prescriptions and insurances!